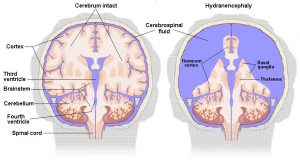
Hydranencephaly is a rare neurological condition in which most of the cerebral hemispheres are absent and replaced with fluid.
Unlike in Anencephaly, which is a defect in brain development, in Hydranencephaly the baby’s brain develops normally until “something” happens to cut off the flow of blood to the baby’s brain or otherwise severely damage it. The affected part of the brain then starts to die and the tissue is resorbed by the body and replaced with cerebral spinal fluid (CSF). The “something” that starts this process can be quite brief. Some of the most common causes are a stroke in the baby, prenatal drug exposure, and the death of a twin in utero. In many of the children the cause is unknown. The damage to the brain usually occurs in the 2nd or 3rd trimester of pregnancy and can occur up to a year after birth as well.
While the damage to the hemispheres is typically extensive, the child’s brainstem is usually (but not always) intact. Since in our experience there does not seem to be any clear relationship between what remains of the hemispheres and the abilities of our children, it seems that they rely largely on their brainstems for relating to their surroundings, for expressing themselves and for their various emotional reactions. Given the highly sophisticated neural mechanisms housed in the brainstem, this is not as surprising as it might seem at first blush. Although it is often thought that someone has to have a cortex in order to be aware and interact with their environment children with Hydranencephaly prove otherwise.
A newborn with Hydranencephaly will look like any other newborn. Their heads may be somewhat enlarged due to Hydrocephalus (a buildup of fluid pressure in the skull) but Microcephaly (small head) may also occur. In some cases Hydranencephaly may not be diagnosed for several weeks or months. It can also be diagnosed fairly accurately in utero.
As time goes on, a child with Hydranencephaly may exhibit irritability, feeding difficulties such as gastro esophageal reflux, difficulty with swallowing or sucking, seizures and increased muscle tone. The first year is often very difficult for a child with Hydranencephaly and many die during this time, while others survive and stabilize. The oldest people we know of with Hydranencephaly are both in their 30s. Some children develop breathing difficulties and may need suctioning and in a few cases children have needed to have a tracheostomy and use a ventilator. Note, however that like other children, no two children with Hydranencephaly are exactly alike. They often differ in how their brain has been affected. Each child develops individually, with different abilities and difficulties which often change over time.
Most of the children we know of can hear and most do so very well, while many are visually impaired. Most of the children with Hydranencephaly know their family members and are very aware of their surroundings. Many can use their hands to play with toys or activate switches. . Most of them are communicatively responsive, and a few of the children can use several words. Children with Hydranencephaly often go to school, go for trips on planes, go swimming, to Disney World, etc. In other words they participate in life as does any other child.
The Brain stem In Hydranencephaly
Basically Hydranencephaly indicates that a child is missing much or most of their cerebral hemispheres, that is, the two masses of folded brain tissue (cortex) that surround the brain stem. Literally “anencephaly” means “without brain”, but this is technically incorrect as a term for the cases to which it is applied, which almost invariably have a brain stem. The brain stem is most definitely a part of the brain, and a very important part of the brain.. However, many children have some of their cerebral hemispheres so can use these and learn to do more than would be expected by this diagnosis. Just as all children are different, all children with Hydranencephaly are different as well. What may be a major difficulty for one child (like seizures) may not even be present in another.
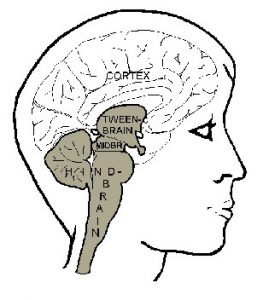
The gray shading indicates the brain stem. It has several parts, each of which includes numerous neural systems with complicated connections with one another. At the top we see the “tweenbrain.” It is more often called the diencephalon, which means the same thing, namely that it is located “between” two other things. What it is sitting between is the brainstem and the cortex, because the whole cortex (the
outer, folded part of the brain) is attached to the brainstem only at the tweenbrain. This means that the tweenbrain is well connected with the cortex, and the part of it, which is particularly, so is called the thalamus, which is the upper part, bulging upwards. The remaining, lower part of the tweenbrain is called the hypothalamus (“below the thalamus”). It is a vital integrating center for hormonal, visceral and motivational regulation. You can see its glandular appendage, the pituitary gland (also called the hypophysis), extending down from it to the right.
The next part of the brainstem is the midbrain, technically known as the mesencephalon. On the left you can see two small bumps. These are the colliculi, or “little hills,” where vision, hearing and the sense of touch are integrated. Below them is a region of neural tissue surrounding a canal called “the aqueduct.” If you look closely the aqueduct is indicated by dotted lines. It carries a fluid – cerebrospinal fluid – which bathes the brain. When the flow of this fluid is obstructed the fluid builds up in the brain, causing hydrocephalus. This must be corrected by a shunt, which allows the fluid to drain. The neural tissue surrounding the aqueduct is called the periaqueductal grey matter, which plays an important role in emotional expression.
Then we come to the large part of the brainstem called the hindbrain. It has several major parts. On the left is the cerebellum, the “little brain.” It got its name because like the cortex it has a folded surface, and looks like a small brain in its own right. It has a role in the adjustment of movement patterns based on learning, and is well connected with both brainstem and cortex. The bulge that you see extending to the right, opposite the cerebellum, is called the pons, the “bridge.” It contains a mass of nerve fibers connecting the cerebellum with itself and the rest of the brain. The border region between the pons and the midbrain houses important systems for regulating cycles of sleep, wakefulness and alertness.
Finally, the lower part of the hindbrain, called the medulla, or “bulb,” extends on into the spinal cord. It contains in a sense the basic wiring of the brain. It houses numerous system – both sensory and motor – which maintain vital functions such as breathing, heart rate and balance and organized reflexes such as swallowing and coughing at an automatic level of functioning.
The above is only a thumb-nail sketch of the most essential parts of the brainstem. With regard to Hydranencephaly it is important to remember that function is determined not only by which parts of the brain are missing and which are present, but also by how the parts that are present are affected by the loss of connections from the parts that are missing. Here there is much that we do not yet know, and some of this we might learn from children with Hydranencephaly.
Dr B. Merker is a neuroscientist in Sweden who is a friend of the families of children with Hydranencephaly.
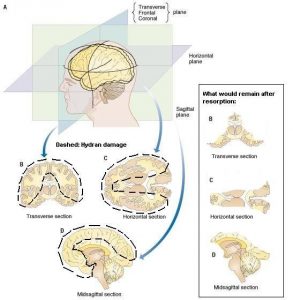
On this page are several diagrams of the brain and what is often remaining in the brain of a child with Hydranencephaly. They are provided by Dr Bjorn Merker. More explanation will be added as time goes on. They are here just to give people an idea of what could be left and what could be missing. Of course all children are different.
Diagrams of the Brain in Hydranencephaly
On this page are several diagrams of the brain and what is often remaining in the brain of a child with Hydranencephaly. They are provided by Dr Bjorn Merker. More explanation will be added as time goes on. They are here just to give people an idea of what could be left and what could be missing. Of course all children are different.
Hydranencephaly Fact Sheet
For many families the first information they find on the internet about Hydranencephaly is this “Fact Sheet” from the National Institute of Neurological Disorders and Strokes.http://www.ninds.nih.gov/disorders/hydranencephaly/hydranencephaly.htm
As a group we have learned that things aren’t always as dismal as stated in the NINDS Fact Sheet and have prepared our own “Fact” Sheet based on our experiences and our informal surveys done over the years.
Please note: Barb Alemán on behalf of the International Hydranencephaly Support Group writes the following information. We are families of children with Hydranencephaly, not physicians. The information is based on our experiences and on the results of several informal surveys*, which we have done. It is meant to be a balance between what information is currently available and what Doctors tell parents. Text in italics are quotes from a variety of sources on the internet.
Description: Hydranencephaly is a rare neurological condition in which the brain’s cerebral hemispheres are absent and replaced by sacs filled with cerebrospinal fluid. (National Institute of Neurological Disorders and Strokes NINDS) The preceding statement is untrue. The correct description of
Hydranencephaly is “Where in ordinary circumstances the cerebral hemispheres fill the meningeal (membranous) linings inside the skull, in hydranencephaly large parts of the cerebral hemispheres are missing. The meninges typically line a normally shaped skull, and cerebrospinal fluid fills the space between remaining parts of the hemispheres and these membranous linings. In some children these linings may detach from inside the skull.”
Others have large sections of such tissue left, for example parts of the cortex along the midline or in the occipital lobe (the cortex at the back of the head). Sometimes the cerebellum and basal ganglia are present and normal. ( http://chorus.rad.mcw.edu/doc/00194.html ).Sometimes they are also missing. Or there are small pockets of brain tissue throughout. Some children also have damage to their brain stem in addition to loss of tissue above the brainstem.
Hydranencephaly is considered to be an extreme form of porencephaly (a rare disorder characterized by a cyst or cavity in the cerebral hemispheres) and may be caused by vascular infections or traumatic disorders after the 12th week of pregnancy. (NINDS)
Cause of Hydranencephaly
In our most recent study (2010), 101 people answered the question, and the cause of their child’s Hydranencephaly was thought to be Prenatal Stroke: 44%, Prenatal drug exposure: 6%, Prenatal infections: 5%, Death of Twin in Utero: 4%, and in 34% the cause was unknown. In two of the children (1%) the damage occurred after birth. Although physicians don’t consider damage after birth to be Hydranencephaly, as their CT scans look the same as the other children, we count them in our numbers.
Children with Hydranencephaly usually appear normal at birth. Sometimes the head is enlarged. “The infants’ head size and spontaneous reflexes such as sucking, swallowing, crying, and moving the arms and legs may all seem normal. However after a few weeks the infant usually becomes irritable and has increased muscle tone. After a few months of life seizures and hydrocephalus (excessive accumulation of cerebrospinal fluid in the brain may develop). (NINDS)
Treatment: There is no definitive treatment for Hydranencephaly. Treatment is symptomatic and supportive. Hydrocephalus may be treated by a shunt (a surgically implanted tube that diverts fluid from one pathway to another).
Hydrocephalus
Hydrocephalus is often one of the first difficulties faced by the child. In our experience 78% of the children have had Hydrocephalus and 96% of those have needed a shunt. Some children have mild hydrocephalus but live their entire life without a shunt and some never do develop an increase in intracranial pressure from fluid.
Irritability
A child with Hydranencephaly is often very irritable in the first year. A build up of fluid in their heads is one of the first things to check if your child is irritable. As 57% of the children have gastro esophageal reflux, which can be very painful this is something that should also be checked. As the children grow older, 90% are said to be happy or quiet. Only 6% were still described as being fussy or irritable past the one year mark.
Increased Tone
Children with Hydranencephaly may have increased tone in their bodies (spasticity). In our study, 41% of the children were described as having increased tone, and 6% were described as being “floppy”. Another 47% were described as having mixed tone. This means that they are sometimes very floppy and sometimes very tight. Physical and Occupational therapy are very helpful in preventing problems from increased tone. However, children do frequently need various orthopedic surgeries as they get older. The therapists will likely suggest a variety of equipment that will also help in preventing a child from developing problems. The children are sometimes referred to as having Cerebral Palsy or Spastic Paralysis.
Seizures
Seizures are fairly common in children with Hydranencephaly (82%). The type and severity of the seizures vary from child to child. Most of the seizures are fairly short and mild but some children do have longer more severe seizures. There are many different seizure medications children take. Often a child needs more than one medication at a time and they frequently need to have their medications changed. A problem both in diagnosing a child who has Hydranencephaly with seizures and in treating them is that EEGs, and medications are geared towards those who are having cortical seizures. Most children with Hydranencephaly have no cortex and have brain stem seizures. So, you and your Dr may agree that your child is having seizures, but nothing shows up on the EEG. And, medications geared at controlling cortical seizures may not work well on a child with Hydranencephaly. That is why your child may need a variety of medications.
Feeding
Children with Hydranencephaly may have trouble sucking and swallowing. Many families are told that their child will lose these abilities within a few weeks of birth when the “higher” cortical areas of the brain normally kick in. We haven’t found this to be true. In our study 33% of the children eat orally, 46% eat only by tube and 19% eat both orally and by tube. As the child gets older he may have more trouble eating and eventually need a feeding tube.
Vision/Hearing
In our study, 91% of the children can hear. Some children may not understand what they hear but do respond to sounds and familiar words. However, parents feel that 30% of the children understand at least some of what is said to them. 63% of the children are thought to see at least some of the time. Most of the children have what is called Cortical Visual Impairment. This means that there is nothing wrong with their eyes, but that their brains aren’t able to tell them what they are seeing. This sort of vision can come and go so that children see some things and not others or will see one day and not the next.
Other Conditions Children with Hydranencephaly may have:
Asthma/Reactive Airways disease (RAD): 34%. Diabetes Insipidus (a high sodium level and excessive urine output): 13% Gastro esophageal Reflux (food comes up which causes vomiting or excessive acid production): 57% . Constipation: 75%